Summary
Objective
The aim of the study was to determine if health-related quality of life of long-term survivors changes 24 months after intensive care treatment compared to the quality of life before admission.
Methods
From 281 patients treated at the ICU in 2001, 132 survivors were contacted by phone on average 24 months after discharge. Fernandez questionnaire was used to assess preadmission quality of life prospectively and postdischarge quality of life, retrospectively. In addition, age, sex, admission diagnosis, ICU length of stay, presence of organ failure, and necessity of mechanical ventilation were determined.
Results
In the 101 ICU survivors who responded to the questionnaire, the total score of quality of life did not change significantly over time (5.48 ± 5.3 before admission vs. 5.6 ± 5.8 at follow-up; p = 0.9). Similarly, the performance of normal daily activities did not alter (3.0 ± 3.5 vs. 3.39 ± 3.6; p = 0,3). In contrast, the ability to perform basic physiological activities worsened significantly (0.39 ± 0.76 vs. 0.76 ± 1.52; p = 0.037), whereas the emotional state improved significantly after intensive care treatment (2.08 ± 1.78 vs. 1.46 ± 1.56, p = 0.003). In a stepwise multiple regression analysis the total score of quality of life before admission was the only variable which influenced the quality of life 2 years after ICU-stay.
Conclusions
In the interviewed population the total score of health-related quality of life did not change after intensive care treatment. Surprisingly, emotional state improved significantly although physical performance decreased. Quality of life after ICU discharge was predominantly influenced by preadmission quality of life. However, these results are not reflective of all ICU survivors.
Zusammenfassung
Ziel
Aufgabe der vorliegenden Untersuchung war es, Verhealth-relader gesundheitsbezogenen Lebensqualität von Langzeitüberlebenden nach intensivmedizinischer Behandlung zu untersuchen.
Methodik
Von 281 an einer internistischen Intensivstation im Jahr 2001 behandelten Patienten wurden 132 Langzeitüberlebende an Hand des Fernandez Fragebogens bezüglich ihrer gesundheitsbezogenen Lebensqualität vor (retrospektiv) und 24 Monate nach (prospektiv) der kritischen Erkrankung telefonisch befragt. Zusätzlich wurden Alter, Geschlecht, Intensivstationsaufenthaltsdauer, Organversagen und Notwendigkeit einer künstlichen Beatmung erfasst.
Ergebnisse
Bei den 101 Patienten, die die Fragen beantworteten, veränderte sich der Gesamtscore der Lebensqualität nicht signifikant (5,48 ± 5,3 vor vs. 5,6 ± 5,8 2 Jahre nach kritischer Erkrankung; p = 0,9). Ähnlicherweise änderte sich das Ausüben normaler täglicher Aktivitäten nicht (3,0 ± 3,5 vs. 3,39 ± 3,6; p = 0,305). Im Gegensatz dazu verschlechterten sich die physiologischen Grundaktivitäten signifikant (0,39 ± 0,76 vs. 0,76 ± 1,52; p = 0,037), während sich der emotionale Status signifikant verbesserte (2,08 ± 1,78 vs. 1,46 ± 1,56, p = 0,003). In der multiplen Regressionsanalyse beeinflusste die Lebensqualität vor der akuten kritischen Erkrankung als einzige Variable signifikant die Lebensqualität beim 2-Jahres Follow-Up.
Schlussfolgerungen
Der Gesamtscore der gesundheitsbezogenen Lebensqualität änderte sich nicht 2 Jahre nach Therapie an einer internistischen Intensivstation. Überraschenderweise verbesserte sich der emotionale Status trotz Verschlechterung der körperlichen Funktionen. Die Lebensqualität der Langzeitüberlebenden wurde vorwiegend beeinflusst von der Lebensqualität bereits vor Auftreten der intensivpflichtigen Erkrankung. Naturgemäß kann von diesen Daten nicht generell auf alle Langzeitüberlebende von intensivpflichtigen Erkrankungen rückgeschlossen werden.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intensive care medicine is expanding in developed countries. Both, number of intensive care unit (ICU) beds and resource utilization are steadily growing [1]. Currently, the ICU costs account for about 13 % of hospital costs [1]. Further increase can be anticipated in coming years, as the proportion of elderly and comorbid population in industrialized countries is growing [2]. Considering these facts, evaluation of critically ill patients’ outcome is sorely needed. As ICU patients often develop organ failure with persisting disability, mortality alone as outcome parameter seems insufficient. Indeed, many investigators integrate the quality of life (QOL) assessment in the evaluation of patients’ outcome.
Thus, QOL of medical ICU patients has been compared with normative population in several studies [3–15]. The majority of these studies reported significant and clinically relevant decrements of postdischarge QOL of medical ICU patients [3, 4, 6–10, 13–15]. Despite the fact that postdischarge QOL improved during follow-up after dismission, it remained lower than the QOL of the age- and sex-matched general population [3, 4, 12, 15].
Interestingly, medical ICU patients exhibit lower QOL than the matched general population already before admission to ICU [11, 12, 15]. Consequently, to estimate the actual influence of critical illness on patients’ QOL, assessment of preadmission status seems indispensable. The preadmission status is difficult to obtain due to frequent neurologic impairment or unconsciousness of ICU patients. To our knowledge, there are only few studies which investigated QOL before admission to ICU [11, 12, 16–19]. All these studies assessed preadmission QOL retrospectively and most of them used the patient’s next of kin in case the patient could not be interviewed [11, 16–19].
Regarding predictors of QOL, only age and severity of illness were found to be associated with at least some QOL-domains [15]. In the majority of studies, age and severity of illness were both associated with lower score at physical domains [6, 11] and age showed, in addition, association with total QOL [20].
Furthermore, changes in QOL observed in ICU survivors depend qualitatively and quantitatively on admission category [18]. Polytraumatized and ICU patients with multiple organ dysfunction experience significant and clinically relevant deterioration of quality of life after surviving critical illness [11, 18, 21, 22]. On the contrary, patients undergoing scheduled surgery report improvement of QOL after intensive care [18]. Finally, changes in QOL observed in medical ICU patients are controversial. Some investigators reported at least slight deterioration of QOL at follow-up [18, 23]. The others showed only temporary deterioration shortly after discharge with improvement during follow-up and long-term QOL similar or even better than baseline values [12, 15].
Thus, given on one hand only few studies investigating preadmission QOL and on the other hand controversial data regarding changes of QOL in medical ICU patients, we intended to investigate changes in quality of life of ICU survivors on average 24 months after discharge from ICU compared to QOL status before critical illness.
Methods
The study was approved by the local ethics committee. Informed consent was waived due to noninterventional nature of the study. Data management was performed according to Good Scientific Practice.
Patients
Study sample comprised all patients admitted to our ICU between January and December 2001, who survived at least 18 months after discharge from ICU. For patients who had more admissions, we considered only the data of the first admission. All study participants were older than 18 years and all were German speaking. The information on survival status was obtained from national register of deaths for all patients admitted to ICU in 2001. Following information was collected from patient charts on all admissions: age; sex; admission diagnosis; ICU length of stay, severity of illness at admission using Acute Physiology and Chronic Health Evaluation (APACHE) III score; presence of organ failure (as defined in Sepsis-related Organ Failure Assessment (SOFA) score); necessity of mechanical ventilation; and ICU survival.
Setting
The study was conducted at the intensive care unit of the Department of Internal Medicine III, Clinical Division of Gastroenterology and Hepatology, Medical University of Vienna. This ICU is a mainly medical ICU, comprised of eight beds that allow complete invasive and noninvasive monitoring, mechanical ventilation and the use of any apparative devices on every position. The ICU team consists of six physicians (three intensivists and three residents) and 28 male and female nurses. There are 3–4 physicians (at least one intensivist) during day shift and two physicians (one intensivist or senior resident and one junior resident) during night shift and weekend. The nurse/patient ratio is 1:1.5 by day and 1:2 at night. During the last years, there have been on average 300–350 patients admitted per year, with a mean ICU-stay of 8 days.
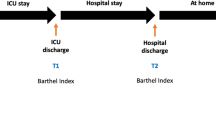
Study design
All patients alive at least 18 months after discharge were contacted by phone by two physicians (VF, PS) on average 24 months after discharge. In case the patient could not be reached the first time, at least three more calls were required, until the patient was declared as drop-out. If the patient could not be interviewed on the phone, the close relative was interviewed instead of the patient. The questionnaire assessed retrospectively the QOL status 2 months before admission to ICU and prospectively the QOL status on average 24 months after discharge from ICU. Both assessments were performed during the same phone interview. Considering potential influence of immediate consequences of severe illness on the postdischarge QOL and the fact that physical sequelae of the critical illness such as critical illness polyneuropathy and myopathy or acute renal failure can improve up to 1 year after discharge, we chose the period of 2 years for follow-up.
Questionnaire
For evaluation of health-related quality of life we used the questionnaire published by Fernandez et al. [24], see appendix. This questionnaire was developed and validated specially for critically ill patients. The test has very good reproducibility and responsiveness [24]. The advantage of this tool is its easy and quick administration, which takes about 5–10 min. Furthermore, the questionnaire can be completed either by patient or by patient’s next of kin—the feature which is very helpful in ICU setting. Finally, the survey can be performed as direct interview or on the phone. The questionnaire contains 15 items grouped into three subscales: basic physiological activities (0–9 points); normal daily activities (0–15 points); and emotional and mental state (0–5 points). The total score ranges between 0 and 29 points, with higher scores indicating lower QOL. The score of 0 points means the best possible QOL, the score of 29 points the worst. The questionnaire was translated into German by forward translation.
Statistical analysis
Metric variables are expressed as mean ± standard deviation (SD). To describe categorical variables the absolute and relative frequency was calculated.
Primary analysis:
The Wilcoxon signed rank sum test for paired data was applied to estimate changes between baseline and follow-up scores for total QOL and for each subscale (performance of basic physiological activities, normal daily activities, and emotional state).
Secondary analyses:
A stepwise regression model was performed to explain the total QOL score 2 years after discharge. As independent factors we used age, sex, preadmission QOL, admission diagnosis (medical/surgical), ICU length of stay, presence of organ failure, and necessity of mechanical ventilation.
To explain the differences in QOL score 2 years after discharge between diagnostic categories (the patients were grouped into five categories: (1) liver disease: liver cirrhosis, acute liver failure, (2) neurologic disease, history of cardiopulmonary resuscitation, (3) cardiovascular disease: heart failure, pulmonary hypertension, (4) infectious and inflammatory disease: sepsis, pneumonia, pancreatitis, and (5) postoperative) an Analysis of Variance (ANOVA) was performed. This was done for the total score, but also for each subscale (performance of basic physiological activities, normal daily activities, and emotional state) separately.
We used the SAS statistical software system (version 9.1, SAS Institute Inc., Cary, NC, USA) for the calculations. In general, two-sided p-value < 0.05 was considered as statistically significant.
Results
Out of 305 admissions to the intensive care unit during 2001, 24 patients experienced readmission, thus, resulting in 281 patients treated at the ICU in this year. Seventy-four percent of the population treated (208 patients) survived until ICU discharge. At the time of questionnaire administration on average 2 years after discharge, 132 patients (47 % of treated patients) were alive according to Austrian national register of deaths. The QOL-assessment could be obtained either directly or indirectly using patient’s next of kin from 101 patients (76.5 % of survivors). No study participant, who could be contacted by phone, refused to complete the QOL questionnaire (100 % response of patients, who were asked to participate in the study). Figure 1 demonstrates a flow diagram of patients’ recruitment.
Demographic and clinical information on the initial cohort (all treated patients), on the QOL—questionnaire responders (analyzed population) and on the patients who could not be reached is presented in Table 1. The mean age of all treated patients was 58 ± 15 years, 164 (58 %) were male, 117 (42 %) female. The mean APACHE III score at admission was 62 ± 31, nonsurvivors had higher scores than survivors (86 ± 31 vs. 53 ± 25, respectively, p < 0,001). The majority of patients was admitted from medical general wards in the hospital (n = 95, 33.8 %) and from the emergency department (n = 83, 29.5 %). The most common reason for admission was pneumonia (n = 43, 15.3 %). For detailed list of admission diagnoses see Table 1. In the course of the ICU stay, most patients developed at least one organ failure (defined as SOFA score ³ 2) with the highest prevalence of respiratory (71 %) and circulatory failure (46 %). One hundred and sixty-one patients (57 %) suffered from multiple organ failure (presence of at least two organ failure). In 7.5 % of the patients noninvasive ventilation was required, whereas intubation and invasive mechanical ventilation were applied in 69 % of the cases. Finally, 9 % of patients were tracheotomized due to anticipated prolonged weaning from ventilator. Renal replacement therapy was performed as intermittent hemodialysis in 4.6 % and as continuous hemodia-/hemofiltration in 5.3 % of the cases. The prevalence of organ failure and related therapeutic interventions is demonstrated in Table 2.
Changes in quality of life
In the interviewed population (101 patients) the total score of the health-related quality of life did not change significantly over time (5.48 ± 5.3 preadmission vs. 5.60 ± 5.8 postdischarge; p = 0.922). The changes between baseline and follow-up QOL observed in particular subscales differed from each other. The subscale I, which summarizes the performance of basic physiological activities such as verbal communication, food intake, or urination and defecation control, deteriorated significantly during follow-up (0.39 ± 0.76 vs. 0.76 ± 1.52; p = 0.037). The subscale II reflects the ability to operate in normal daily life, which includes physical capacity, mobility, occupational activities, and social relationships. This scale revealed no significant change after 24 months (3.0 ± 3.5 vs. 3.39 ± 3.6; p = 0.3). Finally, the subscale III, which explores emotional and mental state of the patients, improved significantly over time (2.08 ± 1.78 vs. 1.46 ± 1.56, p = 0.003). Changes in quality of life are depicted in Fig. 2.
Predictors of quality of life
Multiple regression analysis
To identify predictors of quality of life a stepwise regression analysis was performed. From all tested variables (age, sex, preadmission QOL, admission diagnosis (medical/surgical), ICU length of stay, presence of organ failure, and necessity of mechanical ventilation) the total score before ICU admission was the only variable which entered the model (p = 0.0085, QOL (2 years) = 4.06 + 0.28 preadmission QOL), but we observed only a weak correlation between preadmission QOL and QOL after 2 years (Pearson’s correlation coefficient r = 0.26).
Diagnosis-related differences in QOL
In the ANOVA the factor diagnostic category showed statistically significant influence on patient’s emotional state after 24 months (p = 0.011). The postoperative group had the best scores, whereas patients with liver disease the worst (0,86 ± 1.3 vs. 2.86 ± 2.2, respectively).
All other ANOVAs showed no statistically significant difference between diagnostic categories for the total score (p = 0.107), normal daily activites subscore (p = 0.477) and basic physiological subscore (p = 0.395).
The diagnosis-related differences in QOL after ICU discharge are presented in Table 3.
Discussion
Of the 305 admissions, 132 patients survived at month 24. Regarding the total health-related quality of life of the interviewed survivors (101), no significant change was noted after 24 months. One possible explanation for this result is that the patients with probably the worst QOL after ICU discharge, who therefore not survived 2 years, were not included. Similarly, 31 patients, who survived but could not be reached, may have had lower QOL due to e.g. admission in chronic care facilities. However, the last group was not substantially different from interviewed population regarding age, severity of disease, and ICU length of stay.
Noteworthy, if the subscales were examined separately, significant increase in emotional state in spite of significant decrease in performance of basic physiological activities was found. One could argue that these results are due to recall bias, which occurs perhaps predominantly in subscale emotional state as the other subscales are more objective. Assuming that, the conclusion would be rather that there is only a significant decrease in performance of basic physiological activities in interviewed population. However, it remains interesting that after 24 months the ICU survivors perceived their emotional state as improved compared to the period before ICU. Moreover, similar results reported previously in elderly ICU patients speak for the validity of our data [9, 17, 19, 25]. Thus, the elderly perceived their QOL as good [19, 25] or even improved [17] despite decrement in activities of daily living. Further, critically ill patients, irrespective of age, were as satisfied with their health status as general population even though their health-related QOL was low [10]. Finally, comparisons of ICU patients with general population revealed lower scores at all domains of QOL with exception of emotional and mental state [5, 14, 16, 26]. Therefore, opposite changes in particular subscales compensating each other could alternatively explain unchanged total QOL in the present study. Nevertheless, a very important message of our study is that interviewed ICU patients perceived significantly better emotional condition after ICU stay than before. It convinces of the benefits of critical care and supports its use also in patients, who are not expected to return to their former physical condition.
Preadmission QOL was the only variable related to postdischarge QOL in the multiple regression analysis. The preadmission QOL was also a determinant of the postdischarge QOL and predictor of short-term mortality in the study published by Chelluri et al. [16]. Similarly, the mortality of patients with chronic obstructive pulmonary disease was predominantly influenced by QOL before admission to ICU [23]. Thus, our study, in agreement with published data [16, 23], emphasizes the relevance of preadmission QOL.
There is evidence that changes of QOL observed in ICU survivors depend on diagnosis prompting ICU admission [9, 18]. In the present study significant differences between the diagnostic groups were observed only for the subscale emotional state. Not surprisingly, postoperative patients had the best subjective well-being. Generally, patients undergoing scheduled surgery recover faster than other patient groups. In the present study, the postoperative group had shorter mean length of stay than other diagnostic groups, with exception of liver disease. Furthermore, operated patients had the lowest mean APACHE III score and the lowest rate of organ failure. Similar results have been previously published by Badia et al. [18]. Interestingly, in the present study patients with liver disease scored worst at the subscale emotional and mental state. Patients with liver cirrhosis are known to have poor health-related quality of life. Marchesini and coworkers reported that cirrhotics scored lower at almost all Medical Outcome Study Short Form 36 (SF-36) domains compared to normative population [27]. The patients with end-stage liver disease often suffer from anorexia, fatigue, sleep disturbance, encephalopathy, muscle cramps, ascites, pruritus, and many more [27, 28]. Considering the fact, that the burden of the chronic illness remains after ICU, it is not surprising that these patients exhibited the worst perceived QOL.
Study limitations
The study has several limitations. First of all, the questionnaire we used was not validated for a German speaking population. However, it was developed specially for critically ill patients, implicating difficulties of QOL assessment in this population [24]. Further, the questionnaire was widely used in the ICU setting in the previous shorter [22, 29] and in its final version [23, 30], which we used in the present study. The rate of returned questionnaires is low or the questionnaires are not completely answered, if they are sent to study participants [18, 31]. Therefore, similar to many authors, we decided to contact the patients by phone [13, 19, 23]. We chose the Fernandez questionnaire as it has a simple and concise structure and was validated for this purpose.
A further limitation of our study is that preadmission QOL was assessed retrospectively on average 24 months after ICU stay. Thus, the recall and selection bias cannot be completely excluded. Preadmission QOL is difficult to estimate. A prospective assessment would have to take place before admission to ICU. However, the patients stay out of reach of the investigators at this time. Therefore, in the previous studies the earliest evaluation of preadmission status was performed soon after admission [11, 12, 16–18]. As direct interview was in most cases impossible, some investigators used proxy rating [11, 16–18]. We decided to assess the preadmission status retrospectively after ICU discharge. This approach may have resulted in underestimation of changes in QOL. However, our results are in agreement with results of some studies, which assessed preadmission QOL early after admission, confirming the value of the present study despite potential bias [16, 17].
Finally, 77 % of survivors at follow-up responded to QOL questionnaire in the current study. On the other hand, up to 37 % of survivors were lost to follow-up in the published studies [10, 26]. This reflects the difficulties by the evaluation of postdischarge QOL. Some survivors can not be localized, whereas other refuse to participate. In the present study we did not manage to localize 23 % of the survivors. However, all contacted patients agreed to participate.
Conclusion
To conclude, the overall health-related quality of life of the interviewed ICU survivors did not change after 24 months. Further, these patients reported improved subjective well-being even though their physical condition decreased. However, these results cannot be generalized for all ICU survivors as many patients died until the assessment was performed and some survivors could not be reached.
References
Halpern NA, Pastores SM, Greenstein RJ. Critical care medicine in the United States 1985–2000: an analysis of bed numbers, use, and costs. Crit Care Med. 2004;32:1254–9.
Angus DC, Barnato AE, Linde-Zwirble WT, et al. Use of intensive care at the end of life in the United States: an epidemiologic study. Crit Care Med. 2004;32:638–43.
Dowdy DW, Eid MP, Dennison CR, et al. Quality of life after acute respiratory distress syndrome: a meta-analysis. Intensive Care Med. 2006;32:1115–24.
Herridge MS, Cheung AM, Tansey CM, et al. One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med. 2003; 348:683–93.
Maynard SE, Whittle J, Chelluri L, Arnold R. Quality of life and dialysis decisions in critically ill patients with acute renal failure. Intensive Care Med. 29; 2003:1589–93.
Pettila V, Kaarlola A, Makelainen A. Health-related quality of life of multiple organ dysfunction patients one year after intensive care. Intensive Care Med. 2000;26:1473–9.
Flaatten H, Kvale R. Survival and quality of life 12 years after ICU. A comparison with the general Norwegian population. Intensive Care Med. 2001;27:1005–11.
Schelling G, Stoll C, Haller M, Briegel J, et al. Health-related quality of life and posttraumatic stress disorder in survivors of the acute respiratory distress syndrome. Crit Care Med. 1998;26:651–9.
Niskanen M, Ruokonen E, Takala J, Rissanen P, Kari A. Quality of life after prolonged intensive care. Crit Care Med. 1999;27:1132–9.
Ahlstrom A, Tallgren M, Peltonen S, Rasanen P, Pettila V. Survival and quality of life of patients requiring acute renal replacement therapy. Intensive Care Med. 2005;31:1222–28.
Wehler M, Geise A, Hadzionerovic D, et al. Health-related quality of life of patients with multiple organ dysfunction: individual changes and comparison with normative population. Crit Care Med. 2003;31:1094–1101.
Graf J, Koch M, Dujardin R, Kersten A, Janssens U. Health-related quality of life before, 1 month after, and 9 months after intensive care in medical cardiovascular and pulmonary patients. Crit Care Med. 2003;31:2163–9.
Weinert CR, Gross CR, Kangas JR, Bury CL, Marinelli WA. Health-related quality of life after acute lung injury. Am J Respir Crit Care Med. 1997;156:1120–8.
Cheung AM, Tansey CM, Tomlinson G, et al. Two-year outcomes, health care use, and costs of survivors of acute respiratory distress syndrome. Am J Respir Crit Care Med. 2006;174:538–44.
Dowdy DW, Eid MP, Sedrakyan A, et al. Quality of life in adult survivors of critical illness: a systematic review of the literature. Intensive Care Med. 2005;31:611–20.
Chelluri L, Im KA, Belle SH, et al. Long-term mortality and quality of life after prolonged mechanical ventilation. Crit Care Med. 2004;32:61–9.
Konopad E, Noseworthy TW, Johnston R, Shustack A, Grace M. Quality of life measures before and one year after admission to an intensive care unit. Crit Care Med. 1995;23:1653–9.
Badia X, Diaz-Prieto A, Gorriz MT, et al. Using the EuroQol-5D to measure changes in quality of life 12 months after discharge from an intensive care unit. Intensive Care Med. 2001;27:1901–07.
Montuclard L, Garrouste-Orgeas M, Timsit JF, Misset B, De Jonghe B, Carlet J. Outcome, functional autonomy, and quality of life of elderly patients with a long-term intensive care unit stay. Crit Care Med. 2000;28:3389–95.
Short TG, Buckley TA, Rowbottom MY, Wong E, Oh TE. Long-term outcome and functional health status following intensive care in Hong Kong. Crit Care Med. 1999;27:51–7.
Flaatten H, Ulvik A. Quality of life after intensive care in trauma patients. Minerva Anestesiol. 2006;72:479–81.
Vazquez Mata G, Rivera Fernandez R, Perez Aragon A, et al. Analysis of quality of life in polytraumatized patients two years after discharge from an intensive care unit. J Trauma. 1996;41:326–32.
Rivera-Fernandez R, Navarrete-Navarro P, Fernandez-Mondejar E, Rodriguez-Elvira M, Guerrero-Lopez F, Vazquez-Mata G. Six-year mortality and quality of life in critically ill patients with chronic obstructive pulmonary disease. Crit Care Med. 2006;34:2317–24.
Rivera Fernandez R, Sanchez Cruz, JJ, Vazquez Mata G. Validation of a quality of life questionnaire for critically ill patients. Intensive Care Med. 1996;22:1034–42.
Kaarlola A, Tallgren M, Pettila V. Long-term survival, quality of life, and quality-adjusted life-years among critically ill elderly patients. Crit Care Med. 2006;34:2120–6.
Eddleston JM, White P, Guthrie E. Survival, morbidity, and quality of life after discharge from intensive care. Crit Care Med. 2000;28:2293–9.
Marchesini G, Bianchi G, Amodio P, et al. Factors associated with poor health-related quality of life of patients with cirrhosis. Gastroenterology 2001;120:170–8.
Schuppan D, Afdhal NH. Liver cirrhosis. Lancet 2008;371:838–51.
Vazquez Mata G, Rivera Fernandez R, Gonzalez Carmona A, et al. Factors related to quality of life 12 months after discharge from an intensive care unit. Crit Care Med. 1992;20:1257–62.
Rivera-Fernandez R, Sanchez-Cruz JJ, Abizanda-Campos R, Vazquez-Mata G. Quality of life before intensive care unit admission and its influence on resource utilization and mortality rate. Crit Care Med. 2001;29:1701–9.
Hurel D, Loirat P, Saulnier F, Nicolas F, Brivet F. Quality of life 6 months after intensive care: results of a prospective multicenter study using a generic health status scale and a satisfaction scale. Intensive Care Med. 1997;23:331–7.
Conflict of interest
The authors declare that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Peter Schenk and Joanna Warszawska contributed equally.
Appendix: Health-related Quality of Life Questionnaire [24]
Appendix: Health-related Quality of Life Questionnaire [24]
Subscale 1: Basic physiological activities
Item 1. Oral communication
-
Is there difficulty with speech?
-
0- No
-
1- Yes, a dialog can be held, but with difficulty, due to: softness of voice or faltering speech; short phrases or single words (monosyllables)
-
2- Yes, incoherent speech, either sporadic or permanent
-
3- Yes, no oral communication.
Item 2. Urination control
-
Is there difficulty in controlling urination?
-
0- No
-
1- Yes, sporadically, due to: urinary retention; incontinence
-
2- Yes, permanently, due to: need for urinary catheter or bags.
Item 3. Defecation control
-
Is there difficulty in controlling defecation?
-
0- No
-
1- Yes, due to: ileostomy/colostomy; sporadic incontinence; persistent constipation requiring regular enemas
-
2- Yes, permanent incontinence.
-
Item 4. Intake of foods
-
Is there difficulty in ingesting food?
-
0- No
-
1- Yes. Although feeding is by the mouth, there are difficulties due to: difficulty in swallowing; difficulty in handling cutlery; lack of appetite; rejection of food
-
2- Yes. No feeding by mouth and requires: nutrition by nasogastric tube; parenteral nutrition.
-
Subscale 2: Normal daily activities
Item 5. Movements of precision
-
Can the following movements be carried out?
Pouring a glass of water
Yes
No
Using cutlery
Yes
No
Using a key
Yes
No
Shaving
Yes
No
Sewing
Yes
No
-
0- Can carry out more than 3 activities
-
1- Cannot carry out more than 3 activities.
Item 6. Tolerance of minor effort
-
Can the following activities be carried out?
Go up one floor
Yes
No
Walk two blocks
Yes
No
Carry a full shopping bag, a full brief-case or similar
Yes
No
-
0- Carries out these activities in the same way as before
-
1- Cannot carry out one or more of these activities now, but could before.
Item 7. Tolerance of major effort
-
Can the following activities be carried out?
-
Walking 5 kilometers
-
Running 1 kilometer
-
Going up 4 floors without stopping
-
Practising a sport requiring a high level of physical effort such as football, tennis, swimming, or similar
-
0- Can carry out at least one of these activities
-
1- Can carry out none of these activities.
Item 8. Walking
-
Is there difficulty with walking?
-
0- No
-
1- Yes, walks with help (crutch or people)
-
2- Yes, does not walk, and uses wheelchair
-
3- Yes, is permanently bedridden and depends on others.
Item 9. Mobility
-
Is there difficulty in making normal journeys?
-
0- No, can make all the normal journeys
-
1- Yes, only moves about the immediate locality
-
2- Yes, only moves about the house
-
3- Yes, remains in his/her room.
Item 10. Dressing
-
Does the patient have difficulty in getting dressed?
-
0- No
-
1- Yes, needs some help
-
2- Yes, and is totally dependent on others.
Item 11. Work activities or activities appropriate to age
-
Are there difficulties with the patient’s work?
-
0- No
-
1- Yes. He/she has difficulties, but works as before
-
2- Yes. Works only part-time or has changed to a job requiring minimum effort
-
3- Does not work because of his/her condition.
-
For patients retired due to age, the question is: are there difficulties with the patient’s activities as a retired person?
-
0- No, continues with regular scheduled activities
-
1- Yes, continues with regular scheduled activities but with difficulty
-
2- Yes, activities are no longer regular, and are only sporadic, or have been changed for alternatives requiring less activity
-
3- Yes, and has completely abandoned them.
Item 12. Social relationships
-
Are there difficulties with social relationships?
-
0- No, they continue normally within and outside the family
-
1- Yes, and relationships only continue within the family environment
Subscale 3: Emotional state
Item 13. Subjective well-being
-
How do you normally feel?
-
0- Fine
-
1- Not too bad
-
2- Bad.
Item 14. State of mind
-
How do you normally feel?
-
0- I am happy
-
1- I am sad or I feel like crying some days every week (less than 3 days)
-
2- I am sad or I feel like crying every day of the week (4 or more days).
Item 15: Vitality
-
Do you feel like initiating activities?
-
0- I feel like doing things/starting activities
-
1- I don’t feel like doing anything/nothing interests me.
Rights and permissions
About this article
Cite this article
Schenk, P., Warszawska, J., Fuhrmann, V. et al. Health-related quality of life of long-term survivors of intensive care: changes after intensive care treatment. Wien Klin Wochenschr 124, 624–632 (2012). https://doi.org/10.1007/s00508-012-0224-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-012-0224-z